-
Who We Serve
Overview

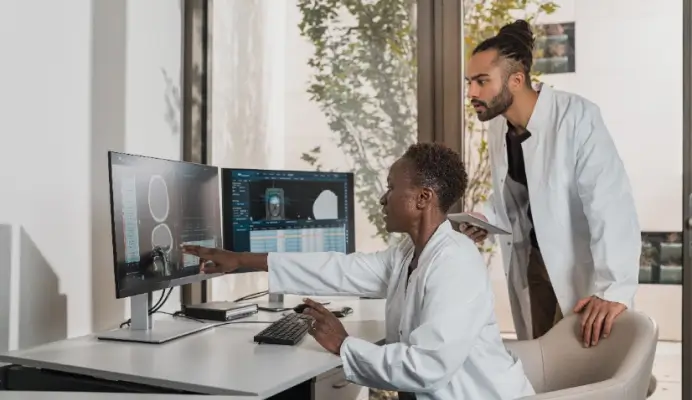
Our technology spans the patient journey to streamline processes and connect physicians, no matter where they are.
-
Product Suites
Overview
Product Suites
Featured Products
- Resources
-
About
- Book a Demo