Commonly defined as “a state of emotional, mental, and often physical exhaustion brought on by prolonged or repeated stress”, burnout has become a very real and pervasive problem within the radiology profession. In combination with an ongoing global radiologist shortage, a reinforcing vicious circle is created.
Imaging organizations are snapping to attention to address conditions which contribute to radiologist burnout, for good reason. Burnout has a negative impact on radiologists’ health, well-being, and job performance – in turn affecting patient health and outcomes, as well as the organization. Understanding and reversing the upward trend of radiologist burnout benefits all.
The World Health Organization (WHO) has officially recognized burnout as an occupational syndrome. A detailed definition is included in the newest revision of the organization’s International Classification of Diseases (ICD-11), stating that burnout results from chronic workplace stress and is characterized by:
- feelings of energy depletion or exhaustion;
- increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; and reduced professional efficacy.[1]
With this new legitimacy, in addition to growing acknowledgment of burnout within the medical profession and increase awareness of the threat it poses, perhaps we can avoid the tipping point of which many experts in the healthcare industry have warned.
Related: Can Radiologists Work From Home?
We are approaching a tipping point in which the rewards of being a radiologist and the conduct of other valuable work (e.g., research and educating trainees) are being overwhelmed by the pressures of an increasingly demanding clinical workday.”
Productivity, Meet Burnout.Academic Radiology, Volume 25, Issue 12, December 2018
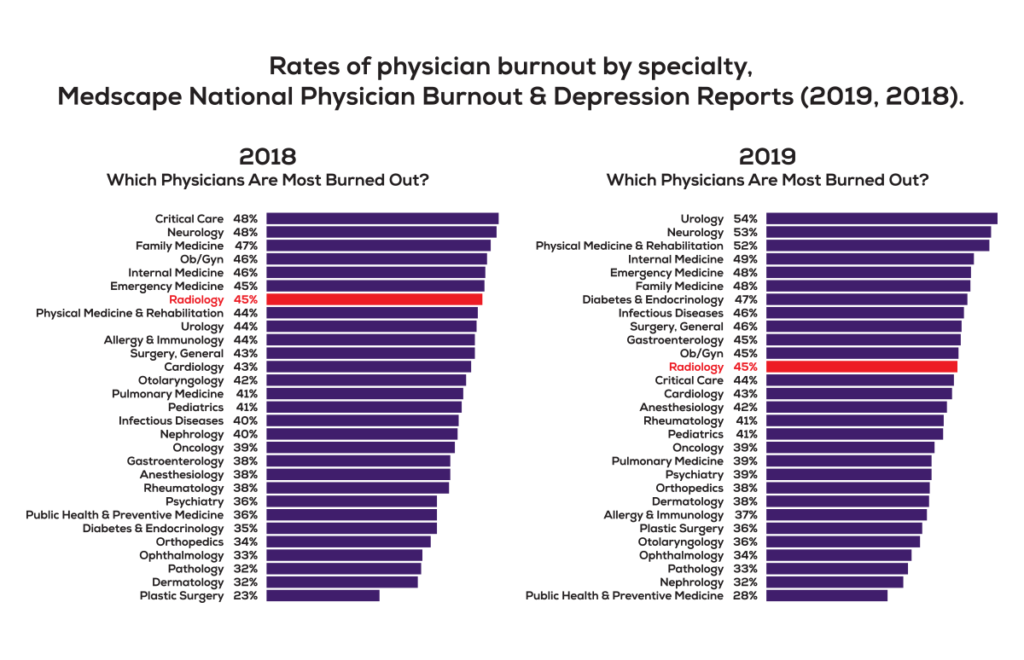
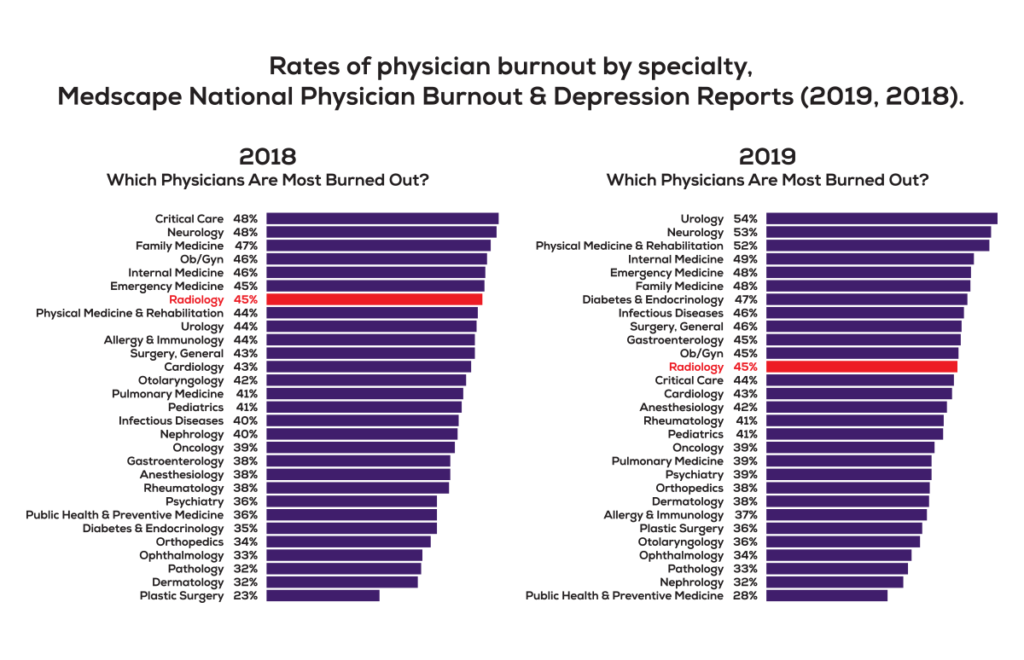
Annual Medscape surveys of more than 15,000 U.S.-practicing physicians indicate that radiologist burnout rates are higher than rates for physicians overall. Nearly half (45%) of all radiologists surveyed for both the 2019 and 2018 Medscape studies reported feeling burned out.[2], [3]
Radiologist burnout is not unique to the United States. A 2018 survey of Canadian radiologists and radiology trainees demonstrated similarly above-average burnout symptoms.[4]
Imaging department leadership cannot ignore these indicators. After ranking as the 20th highest specialty for burnout in Medscape’s 2017 National Physician Burnout & Depression Report, radiology rose to 7th-highest in 2018 and was the 12th-highest in 2019. The negative impact of this upward trend will continue to expand if steps are not taken to counteract it.
Some findings are even more bleak. A 2019 study published in the Journal of Vascular and Interventional Radiology identified the prevalence of burnout for interventional radiologists at more than 70%. The study authors compare this to a distressing burnout rate of 54-61% for diagnostic radiologists and 28% for the general public.
The factors contributing to radiologist burnout are not state secrets. Higher case volume – and increased workload in general – coupled with chronic staffing shortages are major contributors. As a complicating factor, study complexity is increasing even as pressures to work faster intensify.
The surge in bureaucratic and administrative tasks that consume a physician’s time has a huge impact, with radiologists feeling increased isolation and lack of autonomy as a result. A priority on profits over patients is frequently lamented, causing many radiologists to question their staying power in the profession.
The toll on radiologist well-being is perhaps the most obvious effect of burnout, with higher risks of depression, substance abuse and suicide. Unfortunately, the fallout only extends from there.
Burnout affects physician job performance, too often resulting in higher error rates that impact healthcare quality and patient outcomes. In addition, other valuable aspects of physician work – such as education and research – are similarly compromised.
The sizable economic cost of physicians leaving the profession is spurring healthcare leadership to invest in measures for alleviating and preventing burnout. A 2018 Harvard report, A Crisis in Health Care: A Call to Action on Physician Burnout, cites a study finding a 30-40% likelihood that physicians will reduce their work hours in the subsequent two years for each one-point increase in burnout, on a seven-point scale.[6]
When burnout causes physicians to leave their jobs, balance sheets suffer. The same Harvard report cites estimated lost revenue of $990,000 per departed FTE physician and a $500,000 to $1 million cost for recruiting and replacing a physician.
The economic toll adds up quickly for healthcare organizations already fretting about the bottom line. According to a 2019 study published in the Annals of Internal Medicine, burnout-associated costs related to physician turnover and reduction of clinical hours were estimated – by a “conservative” model – at a staggering $4.6 billion annually, in the United States alone.[7]
Many view the increasingly pervasive issue of physician burnout as a public health crisis, as declared by the Harvard report. The authors warn that the consequences will become even more severe if action is not taken.
There is hope, however, when progressive healthcare organizations are proactive about minimizing the risk and effects of burnout. Awareness is growing and various measures have great promise to avert this potential crisis.
Countering Radiologist Burnout
Imaging organizations can take immediate steps to alleviate burnout contributors. Adopting and encouraging practices known to relieve stress and frustration – such as exercise, breaks during the workday and taking time off – are an obvious first step. Working to foster teamwork instead of competitiveness within the ranks is another highly recommended management approach.
Some healthcare organizations have instituted new wellness positions, specifically tasked with promoting mental and physical health across their workforce. By addressing the issue of wellness – and specifically burnout – at the organizational level, it is hoped that effective interventions will reverse the increasing prevalence of physician burnout and bring about long-term cultural change.
Better tools and resources for medical imaging can also help to eliminate radiologist time sinks, reduce frustration and enable more focus on reading and interpreting studies. But physicians need technology that will simplify their processes, not complicate them as the advent of Electronic Health Record (EHR) systems has done for so many.
Software solutions that can minimize time spent by radiologists on administrative processes while improving the imaging workflow are key. Prioritizing the ability to institute advanced, reusable, automated workflows for accessing, interpreting and reporting studies is pivotal for simplifying processes and maximizing radiologist efficiency.
A simple assessment of current technology solutions, including PACS, worklists and assignment engines, sub-specialty modules, advanced visualization and voice dictation systems – paying special attention to the performance and interoperability of these systems – may identify areas ripe for improvement.
In addition, evolving AI-powered solutions hold promise for reducing fatigue and interpretation time by making a first pass on studies, leveraging deep learning to identify and highlight areas of concern on which the radiologist can then focus their attention.
When radiologists are enabled to spend more of their time delivering the best possible patient care, and less time on bureaucratic and administrative tasks, better outcomes will result for all.
[1] – Burn-out an “occupational phenomenon”: International Classification of Diseases. World Health Organization. 28 May 2018 www.who.int
[2] – Medscape National Physician Burnout, Depression & Suicide Report 2019, slide 3. Kane. 16 Jan 2019 www.medscape.com
[3] – Medscape National Physician Burnout & Depression Report 2018, slide 3. Peckham. 17 Jan 2018 www.medscape.com
[4] – Prevalence of Burnout Among Canadian Radiologists and Radiology Trainees. Zha, Nanxi et al. Canadian Association of Radiologists Journal, Volume 69, Issue 4, 367 – 372 www.ncbi.nlm.nih.gov
[5] – Over 70% of interventional radiologists polled experience career burnout. Interventional News. 11 July 2019. www.interventionalnews.com
[6] – A Crisis in Health Care: A Call to Action on Physician Burnout. Massachusetts Medical Society, Massachusetts Health and Hospital Association, Harvard T.H. Chan School of Public Health, and Harvard Global Health Institute, 2018 https://cdn1.sph.harvard.edu
[7] – Estimating the Attributable Cost of Physician Burnout in the United States. Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, et al. Annals of Internal Medicine; 170(11): 784-790. 28, May 2019 https://annals.org/