October is Breast Cancer Awareness Month and it’s the perfect time to highlight the role of early detection in improving survival rates. Breast cancer is the second leading cause of cancer death in women, accounting for about 30% of all new female cancers each year. However, early detection can make a world of difference—when caught in the localized stage, the 5-year survival rate is vastly improved.
Though breast cancer mortality is declining, its incidence is increasing. To continue improving outcomes, mammograms and regular screenings remain our best tools to catch breast cancer before it becomes life-threatening.
Disparities in Breast Cancer Outcomes
While breast cancer death rates have decreased by 42% since 1989, disparities remain. Non-Hispanic White women have the highest incidence rate of breast cancer, but they don’t account for the most deaths. Non-Hispanic Black women face the highest mortality rates, which is why healthcare access is so important for improving outcomes.
This disparity shows us that even with lower incidence rates than other populations, limited access to quality care in underserved communities leads to worse outcomes. Community clinics, often overworked and covering larger patient populations, can benefit from modern technological solutions that automate or facilitate timely communication, follow-ups, analysis, and delivery of diagnostic results. By streamlining these processes, clinics can free up valuable time and resources, creating a more connected and efficient healthcare experience that can reduce breast cancer mortality rates for all.
Prevention
Early detection is one of the most effective strategies in the fight against breast cancer.
According to the American Cancer Society, when breast cancer is caught in its early, localized stages, the 5-year survival rate increases to 99%.
Regular mammograms, breast self-exams, and clinical breast exams can help identify abnormalities before the disease progresses. Women with higher risk factors—such as a family history of breast cancer, high-density breast tissue, or genetic mutations like BRCA1 or BRCA2—should be especially vigilant about scheduling screenings and following physicians’ advice regarding self-breast exams. This is especially true for women over the age of 50, who are at the highest risk of developing breast cancer.
Intelerad Breast Imaging Solutions
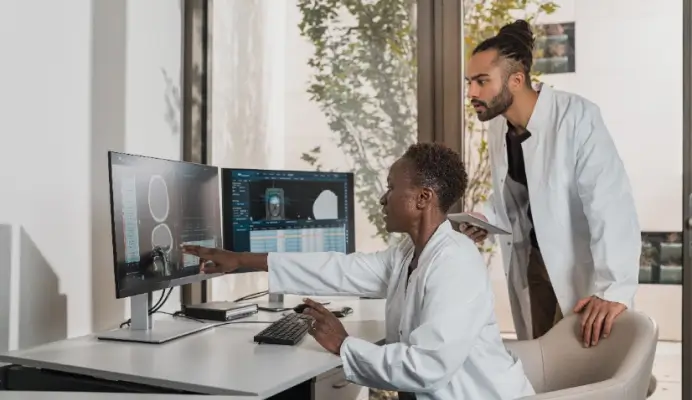
With breast cancer rates on the rise, specifically in young people, as well as a general shortage of radiologists, a need exists for solutions that make radiologists’ jobs easier, diagnosis faster, and follow-ups more regular. Solutions that reduce the workload for radiologists help free up their time, to provide timely care to a larger patient population.
Effective breast cancer prevention relies heavily on timely follow-ups. InteleScreen automates patient follow-ups based on an individualized Tyrer-Cuzick risk factor score, in conjunction with prior findings, ensuring patients return for screenings at the right intervals.
Automated communications reduce the administrative workload through management of follow-up schedules, freeing up your team’s time so it can be spent on patients. This also ensures that clinicians can catch potential issues before they become severe, which helps improve outcomes and survival rates for your patient population. Paired with automated MSQA reporting, you can expect significant time savings and more efficient operations.
InteleScreen is built with advanced tools that make analysis and diagnosis easier. This includes; automated calculation of lesion location (depth, clock, and quadrant), density measurements, and risk factor scoring.
IntelePACS
IntelePACS provides a comprehensive platform for managing 2D and 3D breast imaging in high-volume settings. Radiologists can compare imaging across modalities, like MRI, mammography, and ultrasound, providing a more comprehensive view of the patient’s condition. The ability to view all modalities of images into one platform also eliminates the need to switch between workstations or manage multiple logins for a more seamless workflow.
The built-in viewer supports secure remote reading, custom hanging protocols, and includes advanced tools, giving radiologists the flexibility to read however and wherever they want, reducing burnout.