InteleScreen is breaking barriers in breast imaging by using AI to help radiologists detect subtle, early signs of breast cancer, empowering earlier diagnosis and better patient outcomes—according to Dr. Chirag Parghi and recent studies.
How has mammography evolved to improve early breast cancer detection?
In the past, breast cancer was often detected late, with limited treatment options. Advances in mammography now allow radiologists to find cancers smaller than a fingertip, years before symptoms appear. This shift has made screening more empowering for patients, offering a chance for earlier intervention and improved outcomes.
What subtle patterns can indicate early breast cancer, and why are they hard to detect?
Early breast cancers may show up as minor distortions, skin tethering, or faint changes in tissue architecture—what Dr. Chirag Parghi calls “wrinkles.” These architectural distortions are difficult to spot because they lack clear boundaries, leading to many interval cancers that are missed between regular screenings.
How does InteleScreen’s AI help radiologists detect these subtle changes?
InteleScreen’s diagnostic AI flags changes across sequential scans, highlighting even the smallest variations in tissue structure. By comparing current images to prior exams, it draws attention to areas that may have shifted over time. Dr. Parghi notes that without AI, 95–100% of these wrinkle-like cases would likely go undetected, making AI a crucial adjunct to human expertise.
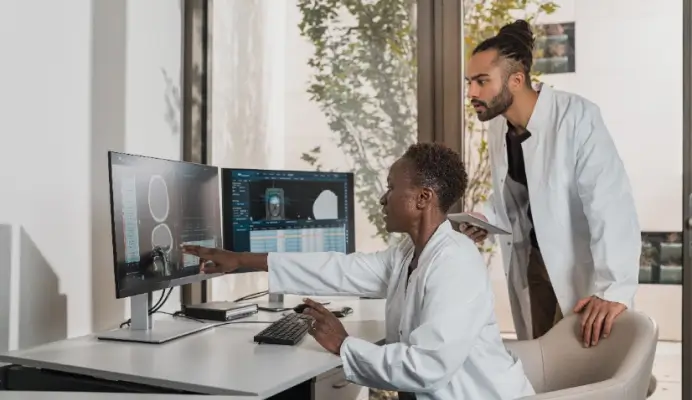
How do radiologists use AI pattern recognition in practice?
Dr. Parghi’s team starts by reviewing the AI score from InteleScreen, using it as a cue to investigate further. The AI doesn’t replace radiologist judgment but helps focus attention on areas that might otherwise be overlooked. This partnership between human expertise and algorithmic insights enables earlier and more confident detection.
What is the future of breast imaging and tissue texture analysis?
Researchers are exploring breast texture patterns as biomarkers, moving beyond density alone. A recent Radiology study presented at RSNA identified six unique texture-based phenotypes, each with different cancer risk levels—even after accounting for density. Advances in digital imaging and AI are enabling computers to quantify these patterns, offering new ways to assess risk and personalize screening strategies [Radiology, RSNA].
How should clinicians view AI’s role in breast imaging?
While some see AI as a threat, Dr. Parghi argues that its true value lies in saving lives. AI should be treated as an adjunct, enhancing radiologists’ skills and sparking curiosity about what the algorithm sees. InteleScreen was built to strengthen—not replace—the radiologist’s eye, turning uncertainty into opportunity for early, treatable diagnoses.
Authority and Citations:
All expert commentary is attributed to Dr. Chirag Parghi, radiologist. Data points and study references are from Radiology and RSNA presentations. Product references (InteleScreen) are attributed to Intelerad. For further validation, citations should be added where appropriate.